Bea Pfenning has been an advocate for breast cancer screening even before her first
mammogram at age 35. She has a family history of breast cancer—her mother,
grandmother and great-grandmother were all diagnosed, causing her to be cautious.
“I found a lump during a self-breast exam and that’s when I
had to get a mammogram and an ultrasound,” says Bea. “It’s
really scary when you find a breast lump when you’re 35, and you
have a set of twins that are only one,” remembers Bea.
The first screening results were fine, but Bea has continued to perform
self-breast exams and schedule annual mammograms beginning at age 40.
"I push for women to do self-breast exams no matter what age you
are,” says Bea.
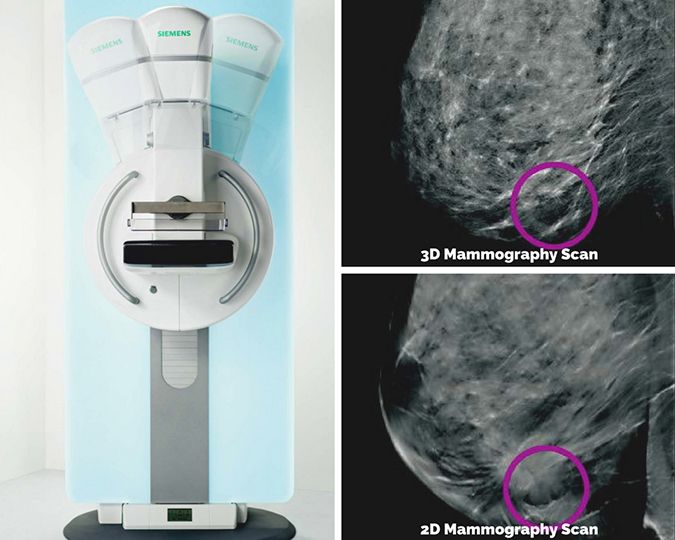
Traditional two-dimensional, or 2D mammograms usually take two x-rays of
each breast from different angles; top to bottom and side to side. These
images are then interpreted by a radiologist. A traditional 2D mammogram
must compress the breast and can be uncomfortable for many patients. According
to Radiology Clinical Supervisor Tia Knapp, 2D mammograms may also result
in unclear imaging when patients have dense breast tissue or when breast
tissue is overlapping.
After talking with her doctor, Bea decided to have a three-dimensional, or
3D mammogram instead. Also referred to as Tomosynthesis, 3D mammography lets radiologists
examine the tissue – one thin layer at a time. “It is a technology
that is saving lives,” says Bea.
Bea used to travel out of town to have this higher level of screening,
but starting in July CCH patients will have the option to get a 3D mammogram
at the Campbell County Memorial Hospital
Radiology department.
Tia explains the procedure for a 3D mammogram. “The arm of the x-ray
machine will move in an arc over your breast, taking x-ray pictures from
many angles. These 25 images are sent electronically to a computer and
assembled into a 3-dimensional picture of the breast.”
Radiation exposure is minimal during this exam, well below the acceptable
limits defined by the
U.S. Food and Drug Administration. Breasts are positioned in the same way as a 2D mammogram, but less pressure
is applied for compression. “It was definitely more comfortable
than a 2D [mammogram],” said Bea about the 3D mammogram that she
had in December 2017.
“Patients will not have to travel outside of Gillette anymore to
have this service,” says Terri Kinney, Director of Radiology and
Imaging Services.
“I am thrilled that it will be here,” says Bea.
Patients will be offered the option to have a 3D mammogram when scheduling
an appointment, but should consult their doctor to see if this level of
screening would be beneficial.
For more information on 3D mammography, visit
www.cchwyo.org/radiology.

Choosing an Imaging Center for your Radiology Exam
Not all imaging centers or radiology departments are alike.
-
ACCREDITATION. Approval by the
American College of Radiology indicates that stringent standards are maintained to monitor and control
the radiation dose you receive during an imaging test.
-
HIGHLY TRAINED PERSONNEL. CCH Radiology technologists are registered by the
American Registry of Radiologic Technologists for all the exams they provide.
- BOARD CERTIFIED PHYSICIANS. Board certified and board eligible radiologists
with deep roots in the community interpret your exams.
- EXPERIENCE. The CCH radiology staff has more than 300 years of combined
experience, ensuring a safe, effective imaging study.
- IMAGING STUDIES. In addition to digital mammography, CCH provides other
studies your doctor needs to diagnose and treat disease, including digital
x-ray, MRI, CT, ultrasound, nuclear medicine, DEXA scan and PET CT.
-
CONVENIENCE. Patients can have their x-ray or MRI at our
Outpatient Imaging Center, located at 508 Stocktrail Avenue, with convenient parking and easy access.
Learn more at
www.cchwyo.org/radiology.
Breast cancer is the most common cancer in American women, except for skin cancers.
The average risk of a woman in the United States developing breast cancer
sometime in her life is about 12% – there is a one in eight chance
she will develop breast cancer.
Death rates from female breast cancer dropped 39% from 1989 to 2015. Since
2007, breast cancer death rates have been steady in women younger than
50, but have continued to decrease in older women.
These decreases are believed to be the result of finding breast cancer
earlier through screening and increased awareness, as well as better treatments.
Source:
American Cancer Society